Today, we will talk about when to Midshaft Humerus Fractures- when & how you decide to operate or not!
Clinical Presentation
- 44 year old male
- History of RTA
- Presented on the day of Injury
- Pain and swelling over right arm
- Paresthesia in distribution of radial nerve; no motor loss
- Co-morbidities – post traumatic neurogenic bladder (Old trauma)

Conservative treatment- When/How/Where to avoid?
Indications
Criteria for acceptable alignment include:
< 20° anterior angulation
< 30° varus/valgus angulation
< 3 cm shortening
Resulting shortening and varus angulation is well adjusted in upper limb and without cosmetic issues.
Method- reduction in GA and cast application/ Coaptation splints
Absolute contraindications
- Brachial plexus injury
- Vascular injury requiring repair
- Severe soft tissue injury or bone loss
Relative contraindications
- Associated ipsilateral forearm fracture/lower extremity fracture
- Pathologic fractures
- Soft tissue injury that hinders bracing
- Iatrogenic nerve injury while attempted reduction
- Bilateral humeral fracture
- Obese patient- difficult to reduce and maintain reduction; compliance issue with brace
- Fracture characteristics
- Distraction at fracture site
- Transverse or short oblique fracture pattern
- Intraarticular extension of fracture line
- Fracture characteristics not in acceptable criteria
Radial nerve palsy alone is not an absolute indication for operative intervention
Absolute indications for fracture fixation
- Open fracture (Compound fractures)
- Vascular injury requiring surgical intervention
- Brachial plexus injury
- Floating elbow
- Compartment syndrome
- Periprosthetic humeral shaft fractures
- Failed Conservative treatment
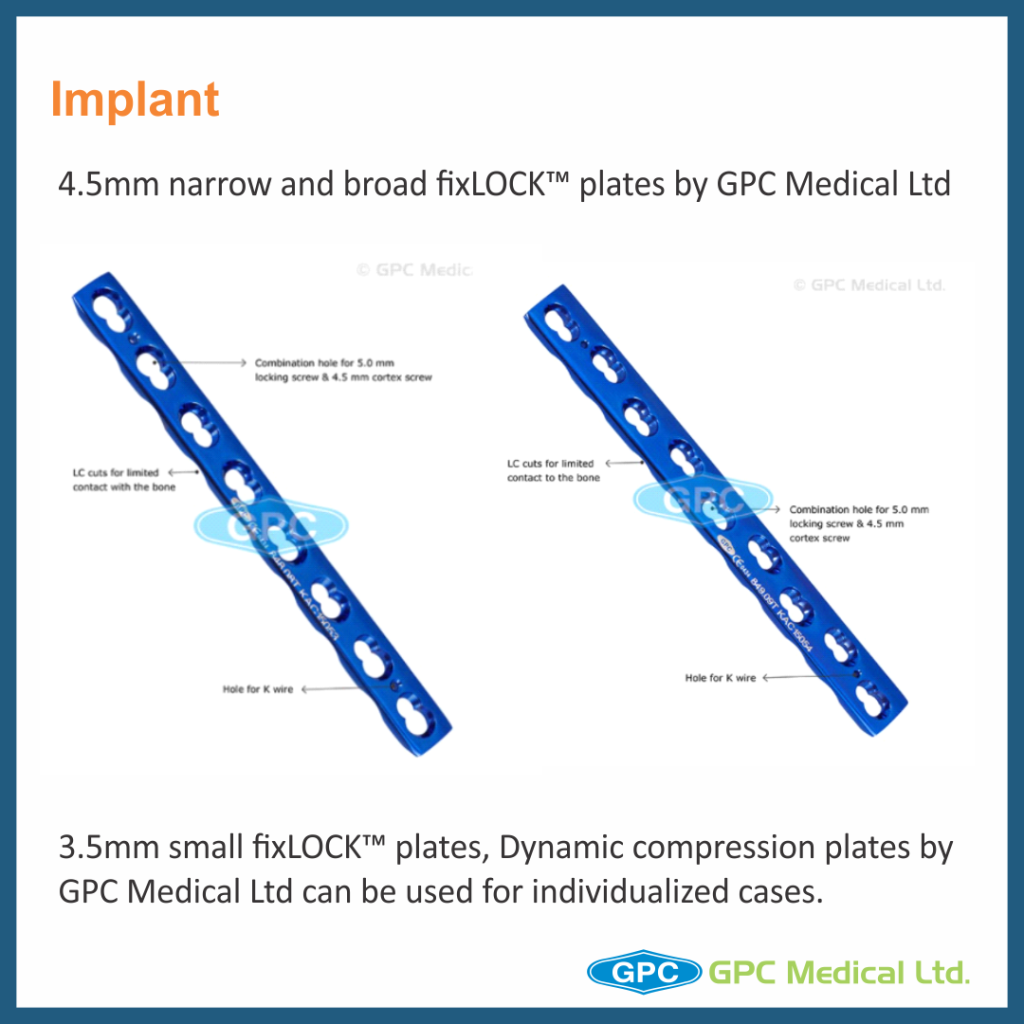
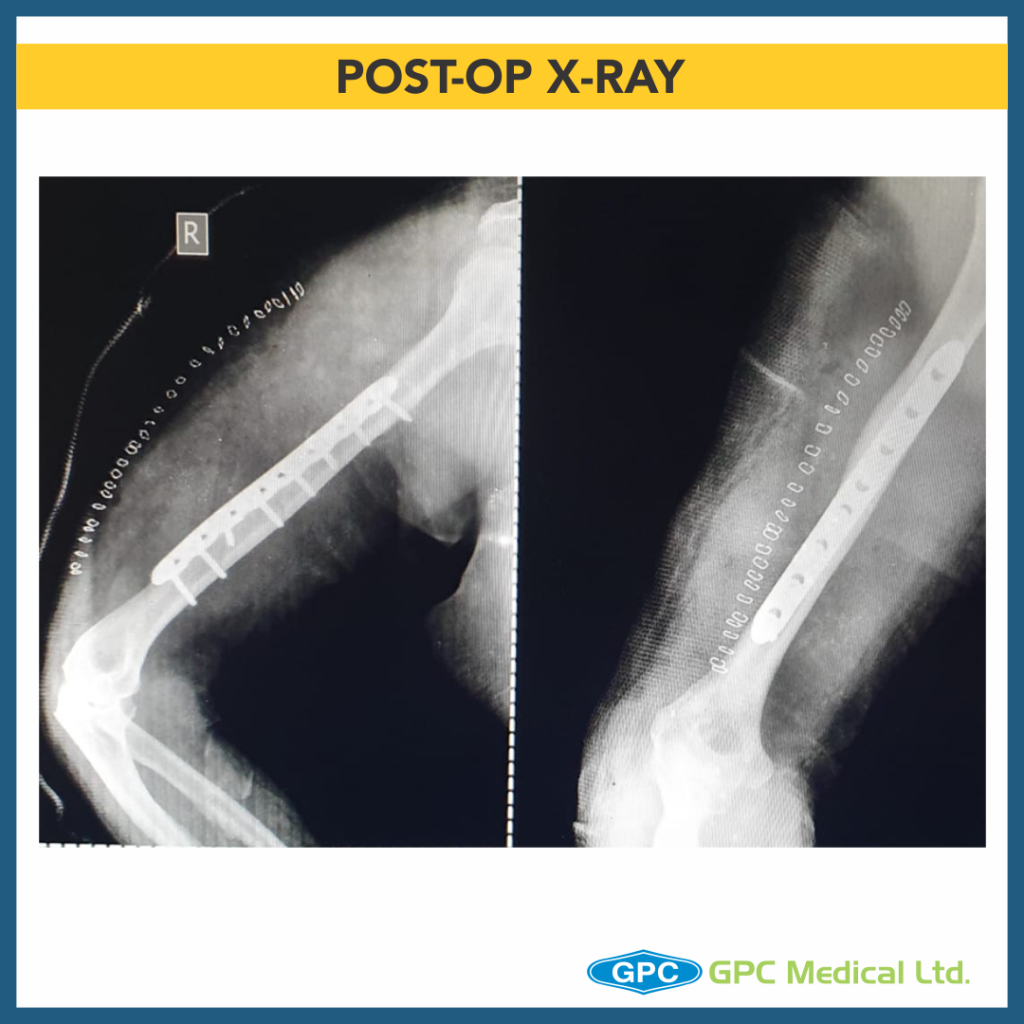
Approach for fixation
- Anterolateral Approach-
- Open with wide dissection
- MIPPO technique
- Proximal third to middle third shaft fractures
- Posterior Approach-
- Distal to middle third shaft fractures
- Cases requiring visualization of radial nerve