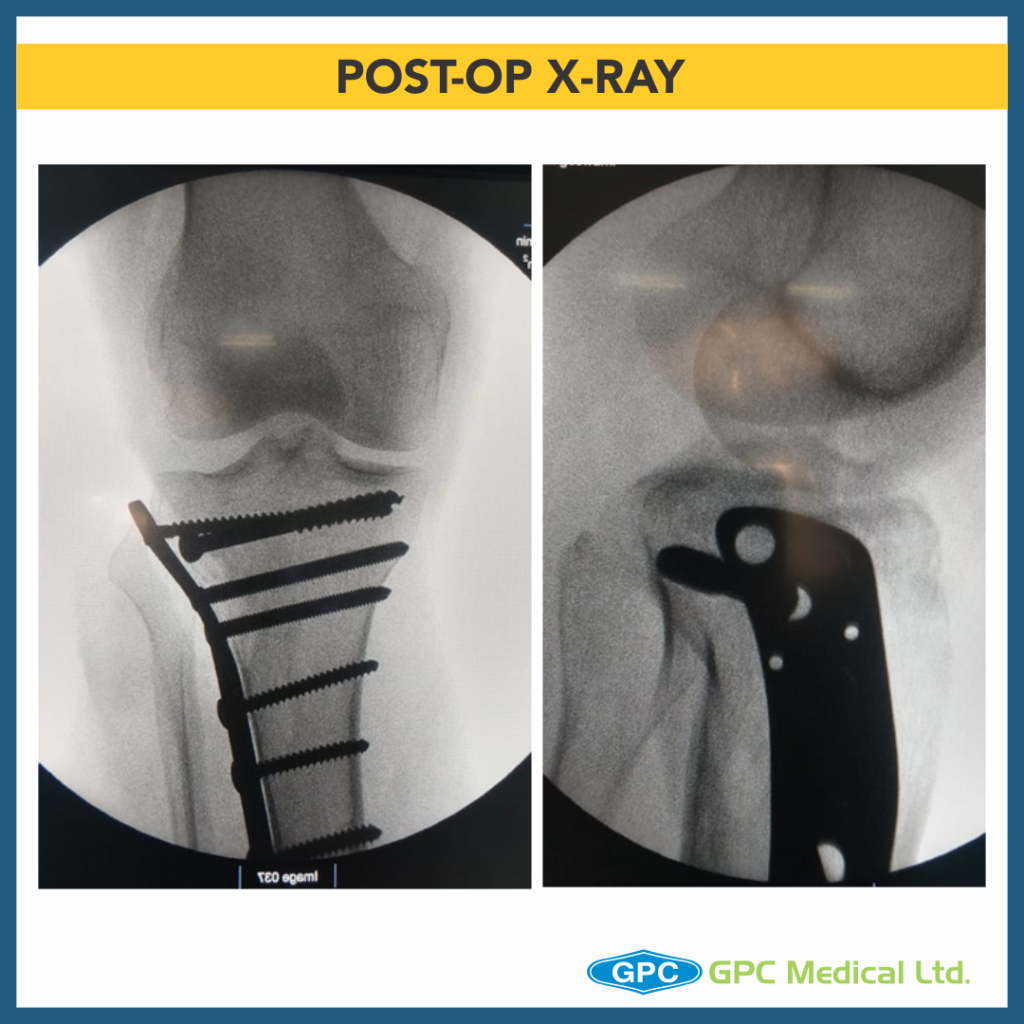
Today, we’re discussing proximal tibia fracture case. Pre-planning is the key! Sometimes for adequate visualisation of the articular surface, surgeons may prefer Arthroscopy, however a few surgeons prefer submeniscal arthrotomy for direct visualisation of fracture reduction.
Clinical History
- 46 year old male
- History of RTA
- Presented on the day of Injury
- Pain and swelling over right leg
- Co-morbidities – nil


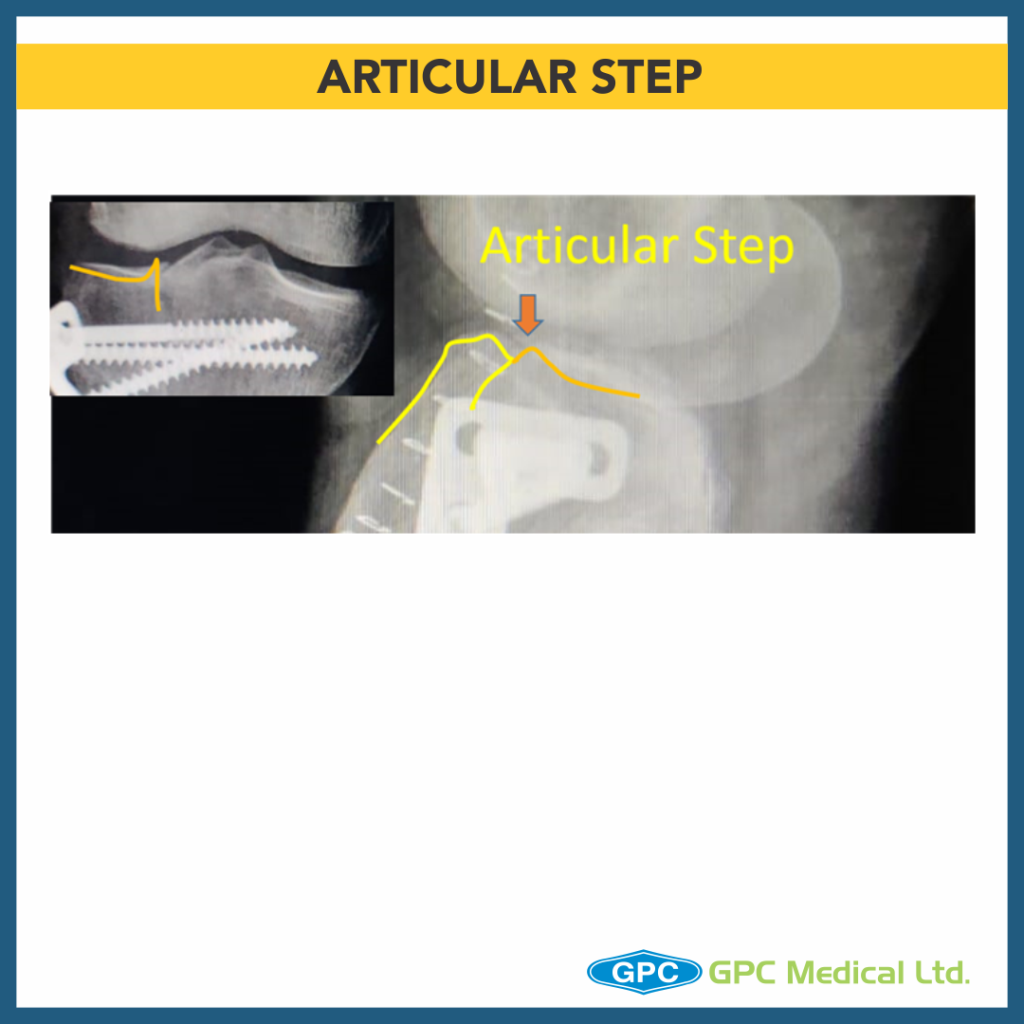
What are the issues with this fixation?
- Fracture appears to be Split fracture of lateral tibial condyle (Schatzker Type 1).
- Articular step has not been corrected.
- Compression not achieved at fracture site.
- Hockey plate gives option of placement of only two screws at subchondral region, additional screws (outside plate) could have been used.
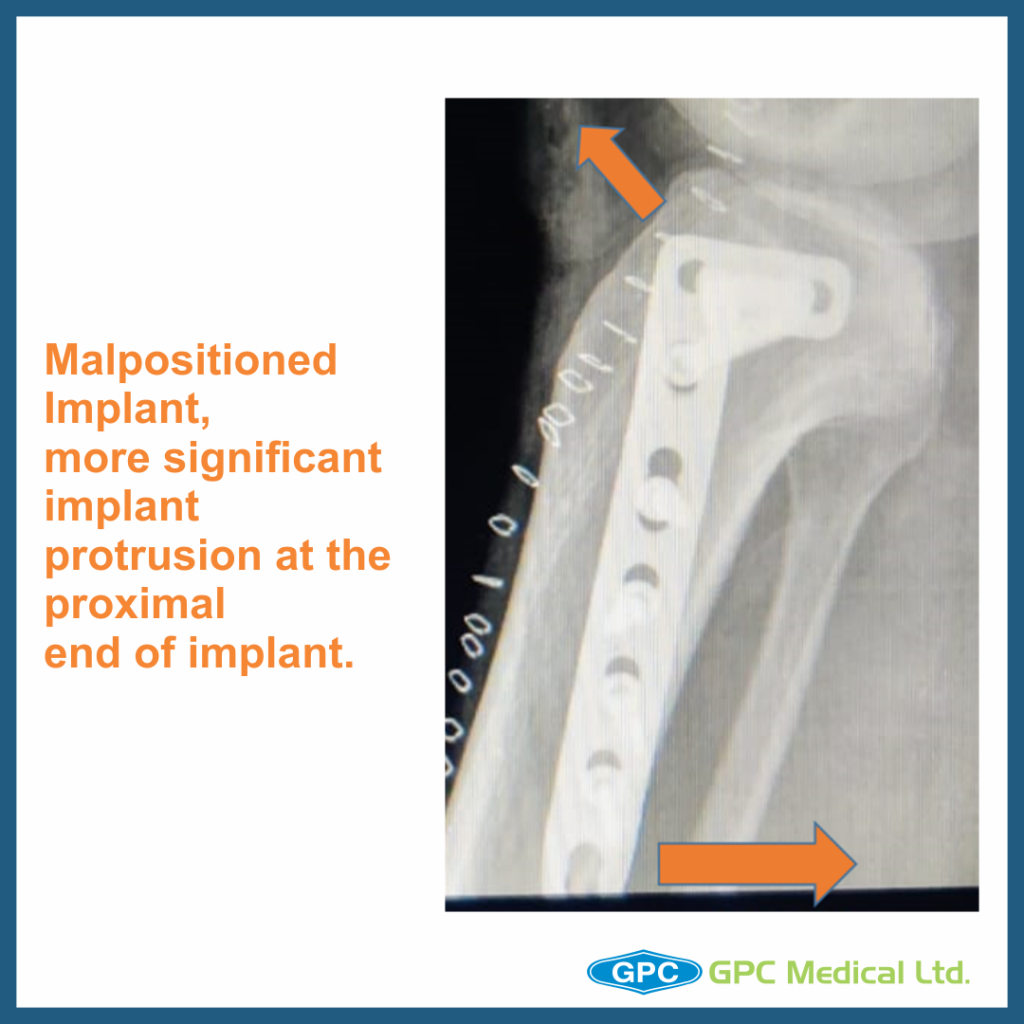
- Plate is not positioned properly can lead to implant prominence.
- Stress riser at plate end due to attempted bone drill.

Which factors led to these issues during fixation?
- Adequate exposure and visualization of the articular surface is of prime importance in fixation of such fractures.
- These fractures require pre-surgical planning in terms of approach required for accessing each fracture with adequate visualization of articular surface.
- Some Surgeons advocate use of arthroscopy to visualize the articular continuity/reduction whereas other group prefer submeniscal arthrotomy for direct visualization of fracture reduction.
- These fractures appear simple and one tends to have minimum visualization of lateral fluoroscopy view in a hurry of fracture fixation.
How to troubleshoot these factors?
- Pre-plan the surgery in-terms of fixation system- Internal fixation/ external fixation.(read implant manual for ideal site of placement of plates)
- Plan the necessary approach.
- Plan for bone grafting if articular depression is observed intraoperatively.
- Always temporarily fix the reduction with K wires/ screw to prevent sagging of articular fragment and Visualize the articular congruity.
- Confirm the fracture reduction in two planes.
- Use of magnified fluoroscopy view of articular surface in anteroposterior and lateral view.
Author approach
- Adequate visualization of the fracture with submeniscal arthrotomy.
- Reduction of fracture and compression is temporarily achieved with condylar compression clamps and temporary fixation with K wires.
- Countersunked Lag screw at the apex of the fracture fragment.
- T shaped plate instead of L shaped Plate as fracture line is in anterior one third tibia(lateral view)
- Longer plate for spacing out screws.
- Backup plan:
- Additional lag screw in condylar region(prior to plate fixation)
- Window on contralateral cortex for elevating articular surface