Today, we are shedding light on a case study of Ulna Bone Fracture. Forearm fractures are common fractures. Here we are talking about when to go for conservative treatment & when to opt for surgical procedure.
Clinical Presentation
- 37 year old male
- History of RTA
- Presented on the day of injury
- Pain and swelling over right forearm
- Co-morbidities – None
- No neuro-vascular deficit
Investigations
- X-ray of the suspected region- pelvis/chest/spine screening/limbs.
- X-ray of affected region- Anteroposterior & Lateral
- Blood workup for surgical fitness

Most common causes of forearm fractures
- Direct impact (Assault)
- Fall on an outstretched arm or fall from a height
- Road traffic accident
Treatment forearm fractures- Surgical
- When to go for conservative treatment?
- Isolated undisplaced fracture
- No associated injury of ipsilateral limb
- No neurovascular compromise
- Treatment modalities
- Muenster cast or olecranon bearing cast
- Functional bracing
Olecranon bearing cast or Functional bracing
- Cast/brace should extend just above elbow to control forearm rotation
- With extension the proximal limit of cast should rest on olecranon process
- High chances of displacement in early stages(check x-ray after 1 week)
- 6-8 weeks of immobilization
- Chances of malunion/nonunion
Surgical Approach
Subcutaneous Approach to Ulnar Shaft
Internervous plane between Extensor carpi ulnaris (ECU) and Flexor carpi ulnaris (FCU) supplied by PIN & ulnar nerve respectively.
Neurovascular structure encountered:
Ulnar vessel and nerve: subperiosteal dissection of FCU as these structure travel under FCU.
Surgical Plan
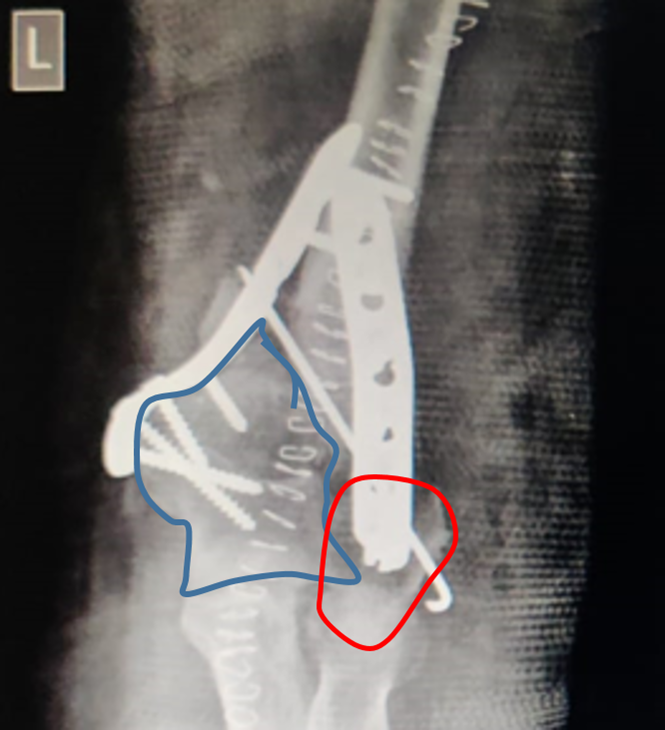
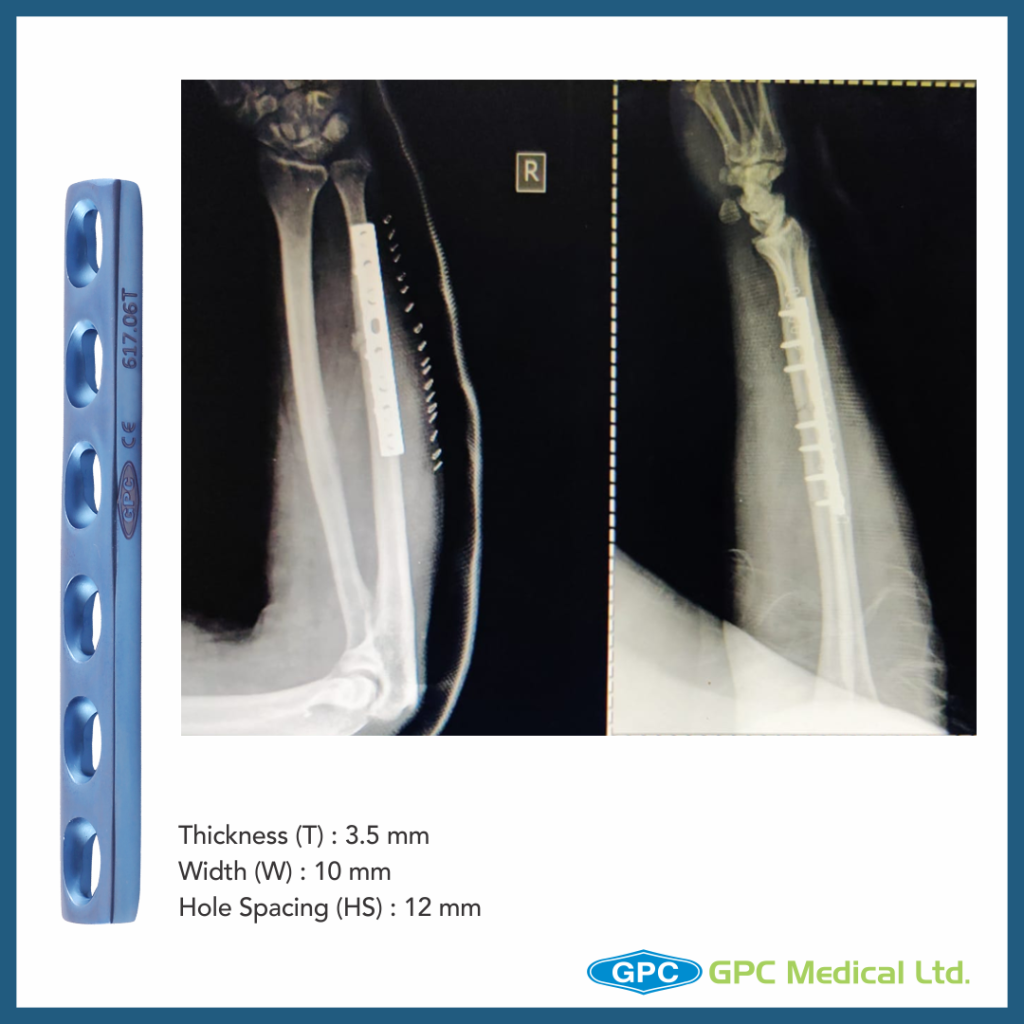
- Implant GPC Medical Ltd.– Dynamic self compression plate for small fragment
- In Anteroposterior view, the fracture is appearing as undisplaced, however in lateral view transverse fracture is seen with butterfly fragment splinting of distal fragment.
- Plan: Position the plate over the butterfly fragment and convert a three fragment fracture to two fragment fracture and achieve compression