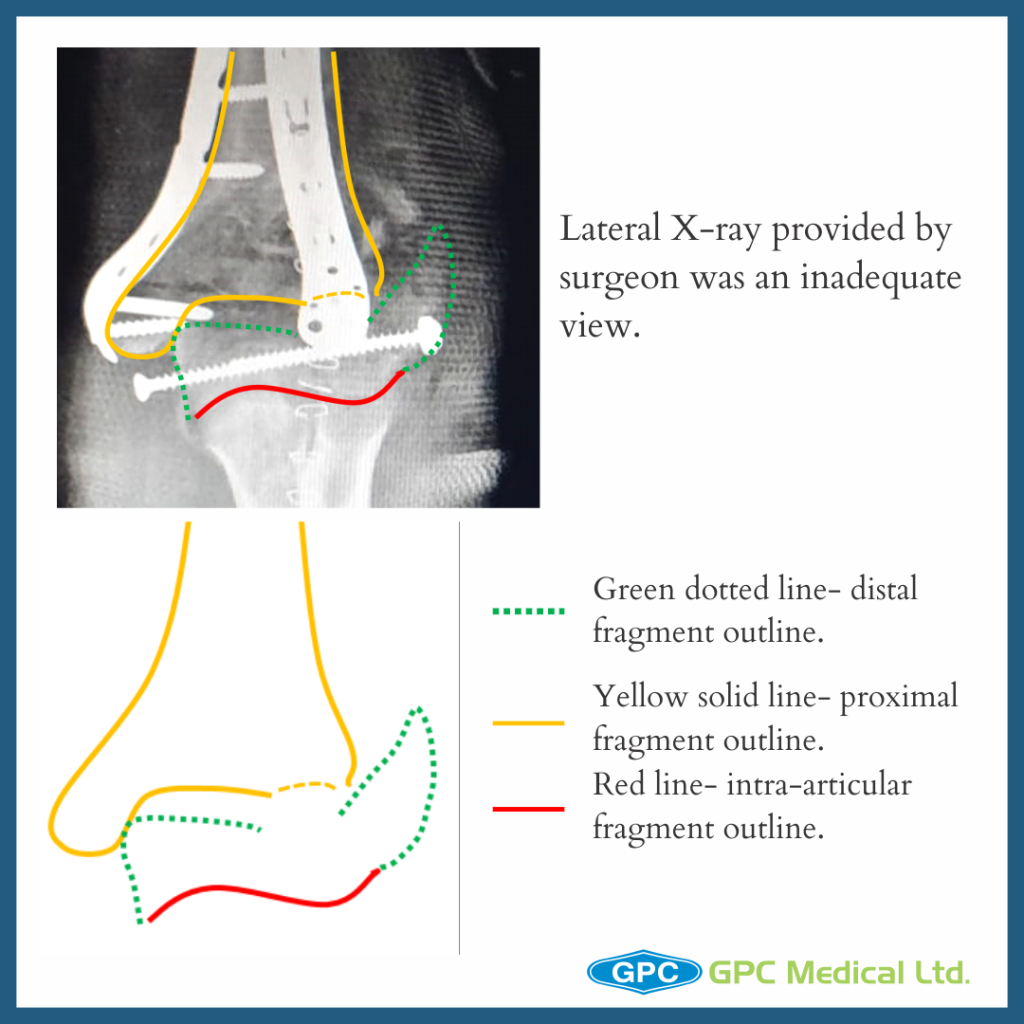
Continuing on last post on elbow reconstruction, today we’re going to talk about the contingency plan i.e. when the surgeon attempted to reconstruct column, but failed to achieve intra-articular fragment reduction.
Clinical Presentation
- 29 year old female
- Thinly built
- Road traffic accident with injury to the left elbow
- Trauma to the skin (abrasion) overlying the fracture
- Closed fracture without any neurovascular deficit
- Co-morbidities – None

Investigations
- X-ray of the suspected region- pelvis/chest/spine screening/limbs
- X-ray of affected region- anteroposterior/ lateral/ traction views (author preference)
- CT scan of elbow (cost constraint)- gold standard
- Blood workup for surgical fitness

What should have been done?
- Author’s preferred method- discussed in one of earlier discussion on distal humerus fractures.
- Simple plan
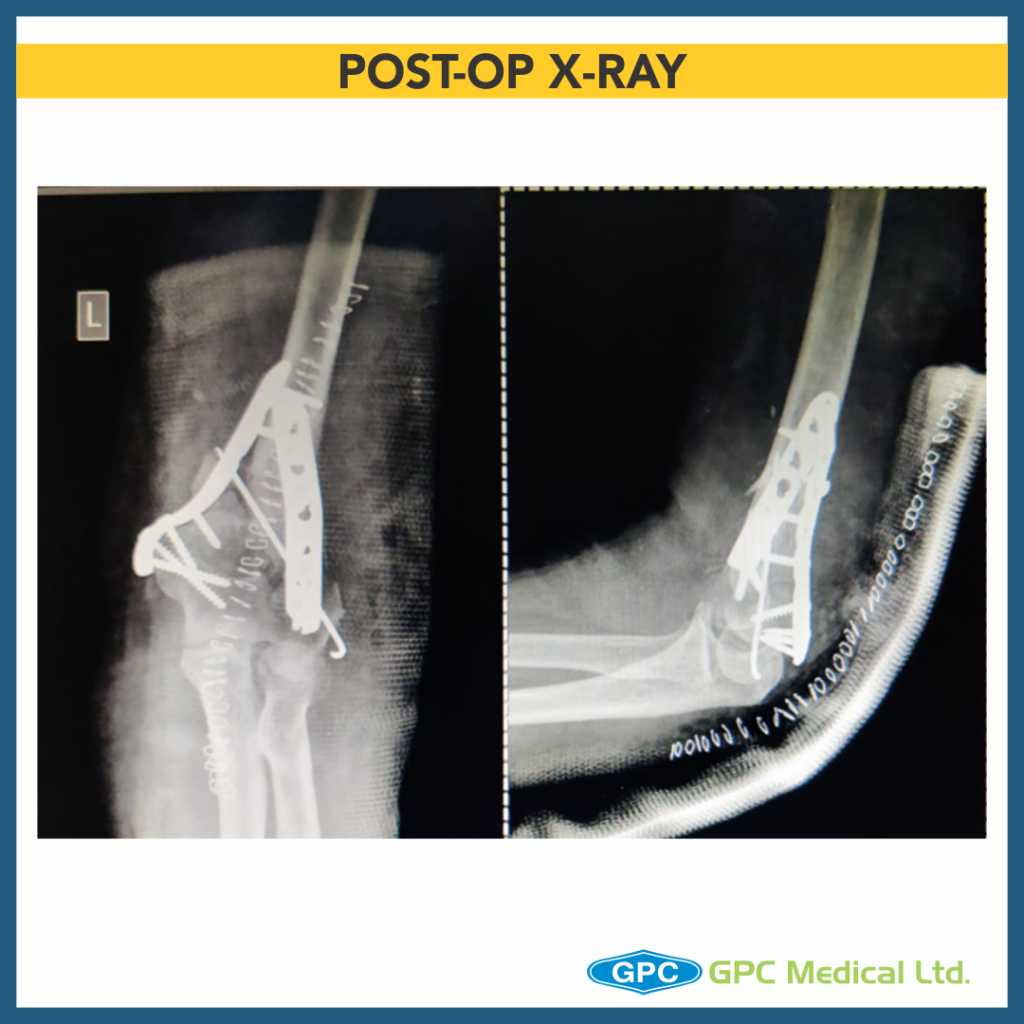
- Olecranon osteotomy
- Intercondylar partially threaded cancellous screw (lag effect)
- Temporary column fixation
- Medial column single screw fixation
- Lateral column fixation by 3.5 mm LCP/Lateral Distal humerus plate

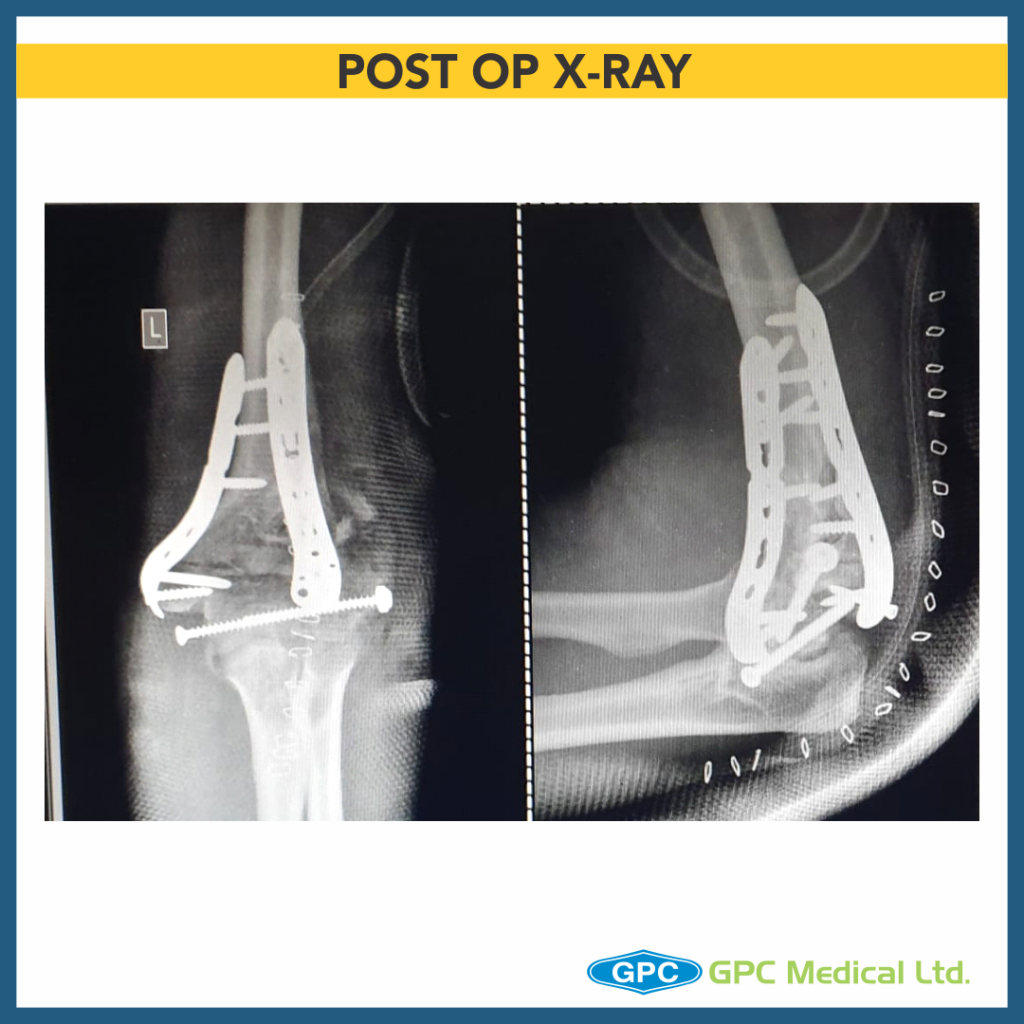
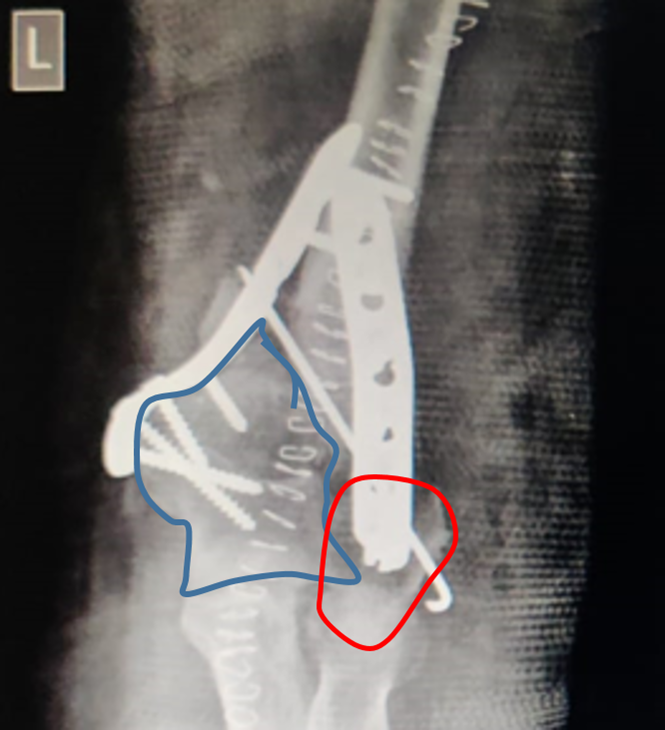
Fixation Issues
- No compression in between two condylar articular fragments
- Medial column not restored
- Anterior angulation of distal humerus not maintained
- Lateral distal fragment- capitullum is fixed in rotation
- Short screw length
- Slab application (length) is not appropriate for such injuries
Why does one land in such issues?
- Pre-op formulate a plan to fix such complex trauma case
- Follow the plan, ensure each step is correctly addressed
- Back-up plan should be there in case difficulty/ problem in original plan (author would have to drop idea of single medial screw and go for medial plate due to comminution)
- Critical analysis of the postop case to ensure adequate results in next case
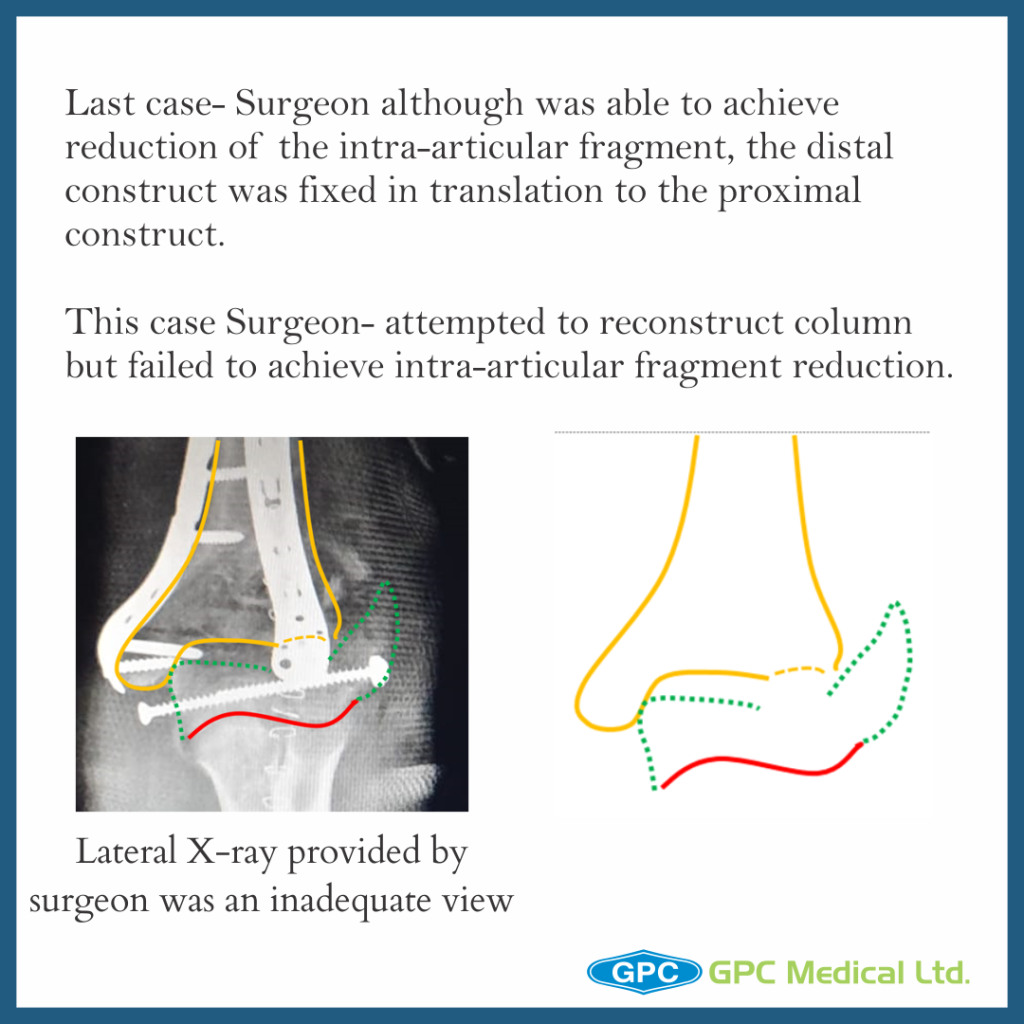
Last Case Discussion
- Pre-op & contingency plan
- Importance of exposure and different methods
- C-arm visualization
- Patient expectancy from injury
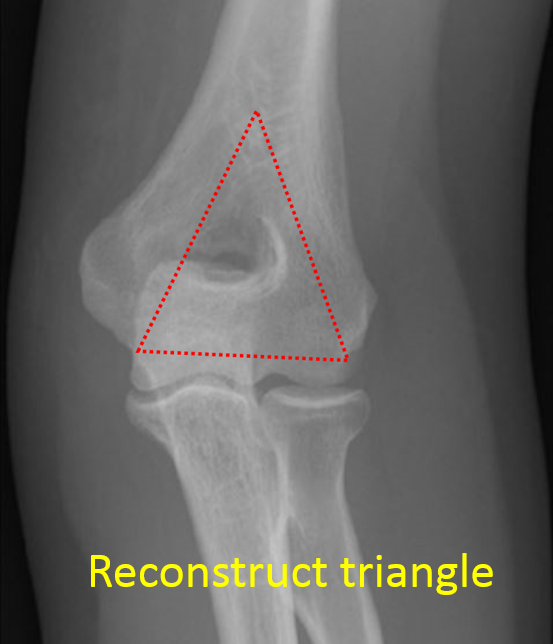
- Strongest bone lies along medial and lateral columns and therefore the implant should be placed here
- Intra-articular anatomical reduction and fixation by lag screw placed from medial to lateral direction
- With normal 40° anterior angulation of the condyles and humeral shaft restored, lateral plate is positioned posteriorly & medial plate in saggital plane along the medial border.
- Screws in the distal fragment need to be as long as possible,engaging as many fracture fragments as possible, ensuring screw tip is not impinging into the joint
- Medial and lateral column screws should “interdigitate“ such that they have hold on opposite column fracture fragment
- Check ROM and fracture fixation stability on the OT table before closure